


Consulting for effective claims management
Horn & Company's expertise in claims management for modern insurance.
Claims management solutions as key success factor
Claims management is one of the greatest levers for customer satisfaction and the profitability of insurance companies. At the same time, this area is not easy to manage due to its highly dynamic nature and fierce competition. As management consultants for insurance companies, our claims experts support you in reducing costs in claims settlement, managing volatility and arrears and optimizing the claims organization. We provide very specific, measurable claims management solutions for our clients. We not only develop solution concepts, but also implement them in full in the claims management systems. In this way, our insurance claims consulting offers a high level of commitment and responsibility to the success of the projects. Examples of past claims projects: Vorgehensmodell zur effektiven und vorausschauenden Schadenregulierung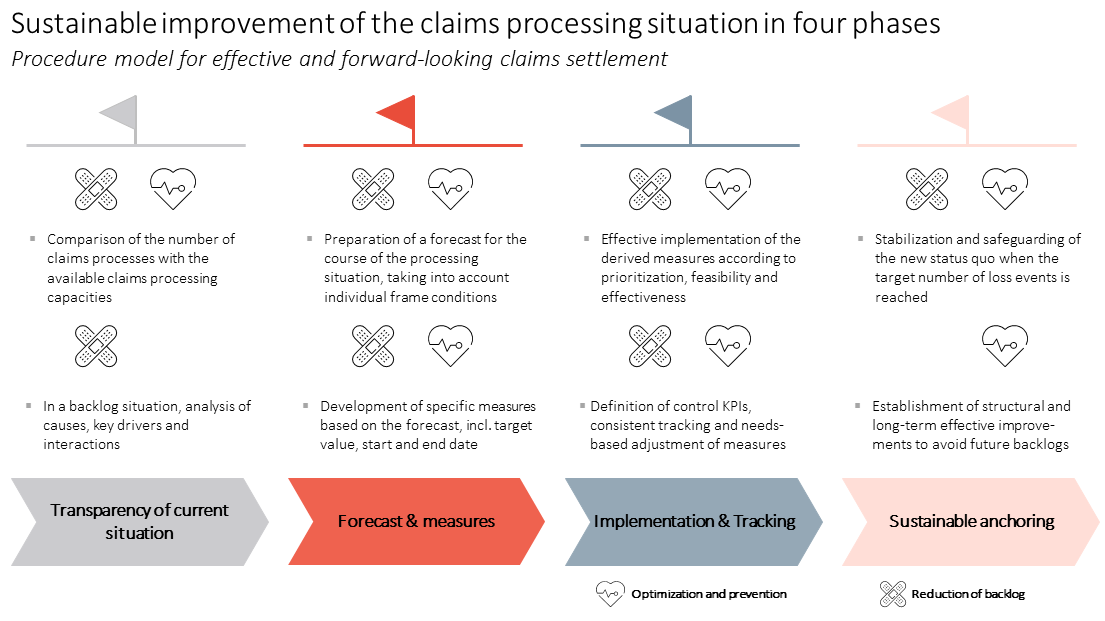
Our experts for effective claims management
Selected references of Claims Management Projects
Reduction of claims expenses for a German property/casualty insurance company
Challenge
Due to a steady increase in claims expenses and declining profitability, our client wanted to reduce claims costs. Therefore, drivers and target savings amounts were defined top-down in a previous strategy project. In a follow-up project, concrete measures should be derived, implemented and the planned savings should be realized. Horn & Company's claims team received the mandate for this project. |
Solution Strategy
The starting point was a bottom-up validation of the previously defined drivers and target savings amounts using business case calculations, expert assessments and benchmark comparisons. The result of the review was that the previously defined drivers were partly not feasible and not sufficient to realize the targeted cost reductions within the claims management systems. In order to achieve the planned savings, the H&C team analyzed the client’s claims management systems in depth and identified additional drivers for compensation. Then, specific measures were developed for each driver. These included, for example, improvements in the cooperation with external service providers for invoice auditing/leak detection, efficiency increases through automation of manual tasks using RPA and claims data analytics as well as optimization of fraud/recourse processes. The claims team then orchestrated the implementation of the measures in several sub-projects. The achievement of the planned cost reductions was secured through benefit tracking and reporting for the management. |
Development of a new operating model for a German health insurance company
Challenge
| The client’s processing of claims was carried out at one level without further differentiation according to customer and efficiency-oriented aspects. Long processing times led to negative feedback from both agents and end customers and ultimately to quality problems in the claims audit services and higher claims costs. |
Solution Strategy
The H&C project team optimized the organizational structure by analyzing and categorizing business transactions. As a result, business transactions were assigned to 1st and 2nd level, both levels were dimensioned appropriately and technical changes (routing) were initiated. These organizational measures were complemented with the definition and implementation of an app strategy to simplify and automate claims processing procedures. Finally, case ownership was established within the claims management systems in order to improve the ability to provide information and customer reference over the entire duration of the claims processing. |
Analysis of customer contact points along the "claims process" and derivation of optimization approaches
Challenge
| Our client faced an increasing backlog in claims processing, largely due to internal follow-up processes that had not yet adapted to changes in customer channel behavior. This led to a high level of manual effort for claims handlers, contributing to inefficiencies. |
Solution Strategy
In the initial phase, the H&C project team conducted a process and volume review to gain a clearer understanding of both customer and insurer channel preferences and usage throughout the claims settlement process. It became evident that follow-up phone calls, prompted by incomplete information from the online claims channel, were causing significant additional workload for the claims management teams. As an immediate solution, the introduction of a revised and streamlined quick claims notification system alleviated pressure on the inbound teams. Subsequently, the issue of missing information was tackled by deploying "smart link" solutions, which further streamlined the process. Following the success of these initial measures, H&C was tasked with developing and conceptualizing a comprehensive new claims and service channel strategy, including an enhanced multi-experience approach for customers. |

